An Alternative Medical Approach – Incretins
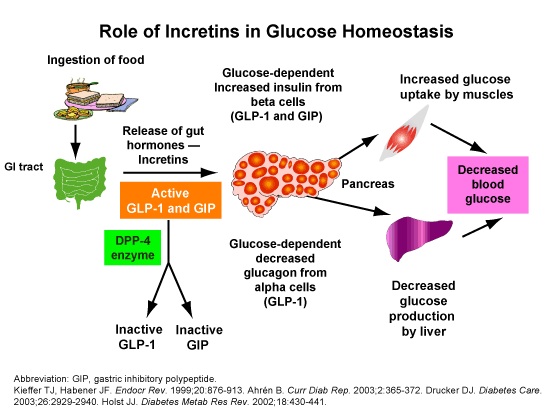
When our stomach releases its contents into the small intestine, the first part of the small intestine is called the duodenum. It totally wraps around the head of the pancreas bringing the duodenal tissue in very close contact with the pancreas. In that area of the duodenum and the jejunum there are very high levels of these entero-endocrine cells that I have been talking about. (Please refer to my previous blogs on this subject if you need the review). These endocrine cells produce hormones that are called incretins. Incretins are the gut derived hormones that stimulate insulin secretion from beta cells after eating. Their primary role is to regulate glucose homeostasis, regulate gut motility, regulate appetite and regulate adiposity. There are two key hormones involved: Glucose Dependant Insulinotropic Polypeptide or GIP and Glucagon like Peptide #1 or GLP-1. If we look at these particular hormones GIP is secreted from cells called K cells. They are mostly in the duodenum and the upper jejunum. GLP-1 incretins are secreted from L cells. These L cells start at the duodenum but they extend all the way to the colon. GLP-1 is quite important in this process.
Does Sugar Always Make it To Our Pancreas?
Many of us, doctors and patients, are of the mistaken assumption that when we eat something that has sugar in it, that sugar gets into our blood stream and eventually finds its way to the pancreas and then we have an insulin response. We now know that that is not fully true. When we eat something that is sweet, those sweet molecules, the fructose or the glucose, interacts with receptors on the L cells or the K cells to release GIP and GLP-1 and the release of those hormones combined accounts for 60% of the insulin that is secreted after a meal. So, the sugar that gets into our blood stream only accounts for about 40% of our insulin response.
Deficient Production of GLP-1
Patients that have long standing Type II diabetes and poor glycemic control are deficient in their production of GLP-1. It is very plausible that these patients that have poor blood glucose regulation have faults in their upper digestive tract and those bitter receptors and the sweet receptors that are regulating the production of the GIP and the GLP-1 may not be doing their thing properly or the L cells may be receiving the signal but are not healthy enough to produce enough GLP-1. We don’t really know the exact picture but we do know that when you give a patient GLP-1 human bioidentical hormone drugs like Exenatide and Liraglutide, which are an injectable delivery system for human identical GLP-1, we see improvements in glucose tolerance. This is a very interesting concept that we can ponder in terms of regulating the health of the cells in the duodenum and the jejunum so that we can produce the GLP-1 appropriately again.
GLP-1
GLP-1 does a few things and we know this from the science and the science has been done around the drugs that I mentioned. GLP-1 increases insulin secretion from the pancreatic beta cells. It suppresses glucagon secretion from pancreatic alpha cells when there is hyperglycemia but not when there is hypoglycemia. This feature means that GLP-1 is going to decrease the production of glucose release from the liver, which is significant. GLP-1 is going to delay gastric emptying, gut motility and this has the downstream effect of delaying the absorption of the ingested sugars and nutrients and that means that our body receives those nutrients more slowly into the blood stream, which make them easier to deal with, another important strategy. It also increases the duration of how full we feel after a meal and therefor suppresses appetite and decreases food intake, which may eventually lead to weight loss. GLP-1 is a very important hormone but the trouble is that it is a very short lived hormone and it is produce in very small amounts and it doesn’t last very long as there are enzymes that break it down. There is another class of drug called Alogliptin which is an enzyme inhibitor to prevent the GLP-1 from being broken down, but of course there are many side effects associated with the use of this drug class because there are many enzymes in our body that are of that same class.
Action in the Pancreas
If we look at the action of GLP-1 at the pancreas we see that it increases the size of the Islets of Langerhans, which are the areas in the pancreas where the beta cells are found, which produces all of these hormones, not just insulin but glucagon as well. GLP-1 also regulates the growth of the Islets of Langerhans and enhances beta cell proliferation and it supports the health of the cells so they have an improved, longer and healthier life span. GLP-1 becomes a very important target when we are looking at optimizing and supporting the patient that needs healthy blood sugar support. When you compare the clinical outcomes using GLP-1 as a therapy they match up very tightly with the observed clinical outcomes with long term Gymnema herbal therapy. So it is my contention that there must be some close relationship between taking Gymnema over a long period of time and some impact on the production or some aspect of GLP-1 biology. This gives us a very strong rational for using the Gymnema herbal over a very long period of time. The dosage with Gymnema is very straight forward. We are looking at 2 – 4 tablets per day for the long term.
GLP-1 & Gymnema
I mentioned that the GLP-1 is released from L cells which are found throughout the entire gastro intestinal tract so Gymnema may be exerting its effect in more than just the upper gastro intestinal tract. When you look at the other aspects of GLP-1, GLP-1 becomes a very important hormone for the trophic benefits across a whole range of cardio vascular and neurological factors. In the large intestine GLP-1 gets produced and that GLP-1 will improve the health of the pancreas, insulin secretion, insulin biosynthesis, help beta cells, help decrease the output of glucose from the liver, and the GLP-1 helps with muscular and adipose tissue insulin sensitivity and stomach emptying. GLP-1 also has a cardio protective function and a vascular protective function as well. With GLP-1 present we observe less atherosclerosis and recent studies show GLP-1 to be neuroprotective. Without enough GLP-1 the brain can’t be healthy.
Watching What You Eat
Our patients that are in this excess blood sugar category get there largely because they don’t have a good diet. When you are eating large amounts of sweet and fatty foods you alter the bacteria in the large intestine and when that happens you end up with dysbiosis. Dysbiosis is known to cause poor health in the linings of our gastro intestinal tract and if you have poor health in the linings of the gastro intestinal tract the L cells won’t produce as much GLP-1 and you will start to lose all of those trophic benefits that I just mentioned. This is a link between the diet and the spectrum that our patients get on when they are in this metabolic diabetic category. I’m not saying that this is the only reason but it is a very interesting insight and very commonly doctors are not dealing well enough with what is happening in the gastro intestinal tract for these patients with these metabolic conditions. We will take a closer look at dysbiosis and the proper application of pre and probiotic therapy in my next blog. It is looking like this will be a 5 part series. I don’t want to lay too much out there at a time because I really want you to get what I am saying here and start looking at sugar management as something doable. All too often I see patients who have resigned themselves to using the medications for the rest of their lives but the risks and probability of serious complication of making that decision are quite inevitable. If dietary correction with proper herbal application is achieved we can look forward to more happy endings. Please stay tuned for Part 4 next week.
